4. Do not leave cat bowls and other personal belongings in places where wild animals can get to them.

- Rabies in cats – symptoms and diagnosis, the danger of the disease to humans
- About Rabies
- A bit of history
- Ways of infection
- How to recognize rabies in a cat
- Identifying symptoms of rabies
- Does a person have to be vaccinated against rabies?
- How can you check an animal for rabies?
- Diagnosis
- There is no cure for rabies
- How rabies is transmitted in cats
- Forms of rabies
- What to do if rabies is suspected?
- Diagnosis
- Sources of rabies
- Risk groups
- How cats get rabies
- Ways of infection
- Symptoms and signs of rabies in cats
Rabies in cats – symptoms and diagnosis, the danger of the disease to humans
There are dangerous diseases transmitted from animals to humans. One of these diseases is rabies – a severe zooanthroponosis infection, ending in 100% fatal outcome for animals.
The disease is transmitted by wild and domestic animals, rodents and birds. Cats, the furry pets of many families, are also highly susceptible to the virus. Rabies in cats can proceed in several forms, so recognize the disease in its early stages is sometimes not possible.
A person becomes infected with the virus through an animal bite – when infected saliva enters the body. Without urgent medical care there is a high probability of death, so if you suspect the cat has the disease, you should limit contact with your four-legged friend.
About Rabies
Rabies (from the Latin Rabies) – Rabies is a highly contagious viral disease of all warm-blooded animals, including humans. Rabies has a mainly acute form and is characterized by complete destruction of the central nervous system.
The disease is widespread, sometimes the rabies virus covers the entire continent. According to statistics, from the disease annually kills more than 50 thousand people and several million animals around the world. Infection occurs after contact with a sick animal. The main sources of the causative agent of rabies are wild and domestic animals.
Wild dogs (wolves and foxes) are in the first place for infection by the virus, cats and dogs are in the second place. It is not uncommon for the disease to be transmitted through the bites of hedgehogs, raccoons, and even bats.
The causative agent is a spherical virus with a diameter of 100-150 millimicrons. Penetrating into a living organism, the pathogen is able to multiply rapidly and accumulate in the gray matter of the brain. In the external environment, the virus is relatively resistant: at minus temperatures the rabies pathogen is preserved for up to 4 months, high temperatures such as boiling kill the infection instantly. Some disinfectants (5% formalin, 5% phenol, 0.1% mercury solution) also kill the virus.
Once in the animal's body the rabies virus rushes through the nerve fibers to the brain area. From the CNS the pathogen enters the salivary glands through the nervous tract, where it begins to actively reproduce. Once a feline rabies infection occurs, the animal becomes infected and transmits the dangerous pathogen to healthy animals and humans through bites.
In rare cases, rabies can be contracted by contact with the saliva of a sick animal on exposed areas of the body with scratches, wounds or other lesions of the skin.
Only regular vaccination of pets can prevent the disease. Kittens begin vaccinating when they reach the age of 3 months. Weak and older animals can be vaccinated once every 2 years. Rabies vaccination of cats with no health problems is carried out annually and is considered a mandatory procedure for all animals.
A bit of history
Cases of rabies infection can be found in ancient documents. The Greek scientist Cornelius Celsus as early as the first century A.D. described a case of "water-borne disease" in a dog. He concluded that its cause was some unexplored virus by that time. Mentions can also be found in treatises from other countries.
The first rabies vaccine was created in 1885 by Louis Pasteur, a French chemist and microbiologist. This man is credited with many scientific works. For example, he laid the foundations for vaccinations against chicken cholera and anthrax, as well as discovering the pasteurization technology that we know of.

The Rabies vaccine created by Pasteur first saved the life of a nine-year-old boy named Josef Meister. He was bitten by an infected dog, and his parents, fearing for his health, brought him to the scientist. Pasteur injected the boy with a vaccine, and he did not fall ill. Surprisingly, despite this case, the lifesaving remedy was not officially recognized until years later.
Ways of infection
The virus is transmitted with the saliva of an infected animal. Blood, urine, and other body fluids are not dangerous. This is due to the fact that once in the body Rabies begins to multiply and move along the nerve fibers located in the intestines, salivary glands, mucous membranes, bypassing the circulatory system. This is why it is extremely difficult to diagnose the disease.
Thus, a cat can become infected with rabies by contact with the saliva of an infected animal. For example, by biting, scratching. In the countryside, the danger increases: it happens that the pet's bowl is in the air, where infected hedgehogs, foxes, dogs and other cats can easily reach. One drop is enough for your pet to become infected with the Rabies virus. Transmission is also possible when cats eat infected rodents.
How to recognize rabies in a cat
Contributor(s): Pippa Elliott, MRCVS. Dr. Elliott, BVMS, MRCVS is a veterinarian with more than 30 years of experience in veterinary surgery and treating companion animals. She graduated from the University of Glasgow in 1987 with a degree in veterinary medicine and surgery. She has worked in the same animal clinic in her hometown for more than 20 years.
Number of sources used in this article: 11. You will find a list of them at the bottom of the page.
About 55-60,000 people die from rabies each year in the world. [1] X Source of information This is most often due to bites from rabies-infected animals. Cats that have not been vaccinated or whose last vaccination has expired can become infected by contact with rabid wild animals. If you yourself have come into contact with a cat that you suspect has rabies, know that you should pay attention to a number of symptoms characteristic of the disease. Be sure to exercise extreme caution if you think a cat might have rabies and do not try to catch a rabid animal yourself. Contact a trapping service, your local animal control station, or even the police.
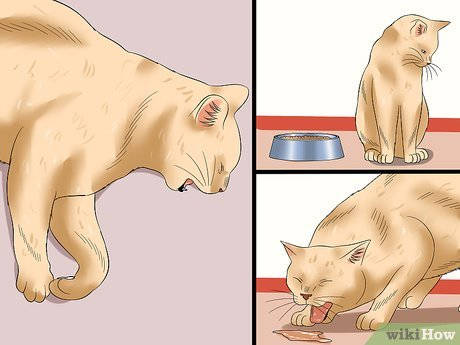
Identifying symptoms of rabies
- Muscle pain;
- restlessness;;
- irritability;
- chills;
- fever;
- general malaise (a painful condition and discomfort);
- photophobia (fear of bright light);
- anorexia (loss of interest in food);
- vomiting;
- diarrhea;
- coughing;
- inability or unwillingness to swallow anything.


- Paralysis (loss of motor function) of the legs, muzzle muscles and other parts of the body;
- droopy lower jaw (which gives the animal a "dorky" look, but it's not funny at all);
- Increased salivation, which leads to foaming around the mouth;
- difficulty swallowing.

- Increased salivation and foaming around the mouth;
- water phobia, expressed as the cat's fear of approaching water and even fear of the noise of water;
- aggression, including grinning, which indicates a willingness to bite;
- restlessness;
- loss of interest in food;
- attacks and biting;
- Inadequate behavior, such as the urge to chew on oneself.
Does a person have to be vaccinated against rabies?
Rabies vaccination is mandatory for pets. Humans do not need to be vaccinated against the disease. If a person is bitten or scratched by an unvaccinated cat, vaccination becomes mandatory. The person may vaccinate if he or she wishes, but this is not required by law.
Vaccinations of domestic cats must be repeated annually. Quality vaccines are used for this purpose. Recently, vaccine manufacturers have begun to make complex preparations that allow you to protect not only against the rabies virus, but also other, no less dangerous diseases. If elderly or weakened animals are involved, it is recommended that rabies vaccination be done separately from all other immunizations so as not to overburden the body.
Vaccination against rabies is carried out only in fully clinically healthy cats. Prior to vaccination, the animal must be treated against fleas, ticks and worms. In most cases, revaccination is carried out every year. The exception is the company Nobivac serum, which guarantees protection against the rabies virus for 3 years. But this is not relevant, because in order to obtain documents from the specialized veterinary public services, you need to be vaccinated annually.
How can you check an animal for rabies?
It is not possible to diagnose rabies while the animal is alive. The only way to check if an unvaccinated animal has been infected with rabies is to quarantine it. Also, in case of emergencies, a mark on the animal's veterinary certificate will help. Diagnosis requires examination of histological preparations of the brain, which makes it impossible to detect the disease in a cat while it is alive.
For safety reasons, suspecting that a domestic cat has come into contact with a wild or other infected animal, it is necessary to place it in a separate room. This should preferably be a carrier. Allowing free contact with a cat suspected of having rabies is prohibited. If the owner suspects that his pet may have contracted rabies, you must immediately inform the veterinary clinic, where the animal will be placed under mandatory quarantine. Trying to care for a sick animal yourself is fraught with serious complications. If a rabid animal scratches or bites a person, the risk of infection is very high. If an animal does scratch or bite, you should wash the affected area with laundry soap and running hot water. After that, you should seek help at the hospital as soon as possible.
Diagnosis
It is impossible to make an accurate diagnosis based on clinical symptoms alone, because the signs of rabies are similar to many severe diseases (e.g., Aujeszky's disease). Some owners believe that the disease can be detected by laboratory blood tests, but this is not true. The rabies virus is not present in the animal's bloodstream, which means that the disease cannot be diagnosed by blood tests alone.
If a pet shows signs consistent with rabies, the first thing to do is to see a veterinarian.
The pet will be placed under a 10-day quarantine period, which may be extended up to 30 days, depending on the epidemiological situation in the area. At the end of the quarantine period, the furry friend dies or remains alive. Only after the cat's death can the presence of the disease be established. The diagnosis of rabies is made on the basis of pathological anatomical changes, clinical and epizootological data. For the diagnosis of rabies the head or brain of a dead animal is also needed. By means of histological analysis, inclusions of Babes-Negri bodies are detected in the cytoplasm of the brain neurons. The detection of these inclusions makes it 100% probable that the cat was infected with rabies.
Autopsy of the corpse of a dead animal reveals hyperemic mucosa of the oral cavity with ulcers and erosions, hemorrhages in the stomach. Autopsy of the skull reveals tense dura mater and edematous soft dura, cerebral gyrus hemorrhages, spinal canal contains large amounts of exudate.
There is no cure for rabies

No effective treatment against the rabies virus has been developed at present.If there are obvious signs of the disease, the animal is to be put to death.
When a dangerous disease is suspected, the cat is immediately isolated in a separate room and any contact with the rest of the family is completely excluded.
In addition, the owner must inform the veterinarian about signs of rabies in the pet, and then the animal is taken into quarantine and placed in a special box. While the cat is in quarantine, it is closely monitored. Veterinarians, for their own safety, also do not carry out any therapeutic measures with the animal.
If the cat has managed to bite the owner, you must immediately wash the bite site with plenty of warm water and laundry soap, and treat the wound with any antiseptic. Then immediately go to a medical facility for treatment. Antirabic serum is effective only during the first 3 days after the bite, if the precious time is missed, the person may die.
How rabies is transmitted in cats
There is no congenital immunity in cats to this disease, it can only be acquired as a result of vaccination.
From the moment the virus enters the body until the appearance of a clear clinical picture always passes a certain time, which is called the incubation (latent) period. Its duration depends on the age of the cat. In adults it can be from three to six weeks, in small kittens – never more than 7 days. The duration of the incubation period also depends on the overall condition of the animal, the depth, size and area of the bite. For example, with bites to the head, the latent period is significantly shorter.
Rabies in domestic cats can have quite different symptoms. The clinical picture will depend on the form of pathology.
Forms of rabies
The violent form is fixed most often, the first signs of rabies in cats in this case are as follows:
- Changes in the animal's behavior – sometimes the cat looks lethargic, avoids contact with people, and has no appetite. And sometimes, on the contrary, the animal behaves too obtrusively and affectionately, constantly resting its head against the owner's legs.
- Increasing feelings of anxiety, increased fearfulness. The cat is constantly scratching and gnawing at the bite site.
- Perversion of appetite – the cat eats common food poorly, but greedily swallows inedible objects (stones, straw, wood chips…).
As the pathology progresses, the main signs of rabies in cats appear:
- Difficulty swallowing, caused by spasms of the smooth muscles of the pharynx, accompanied by profuse secretion of saliva. Sometimes owners think that the animal has choked on something.
- Increased aggression, even to the point of rage – the cat lunges at people and animals. At the same time, these attacks are followed by a state of depression and exhaustion. And at the slightest shout, noise, bright lights, the attack of rage resumes.
- Emaciation and loss of voice.
- Lower jaw drooping, tongue protruding from mouth, accompanied by profuse saliva secretion.
- Strabismus, dilated pupils, sometimes corneal clouding.
In the latter stages of the disease, paralysis of the limbs and torso sets in. On average, the active phase of rabies can last from 3 to 11 days. Death of the animal comes from paralysis of the respiratory and cardiac muscles.
The paralytic (silent) form of rabies lasts for a short time, recognizing rabies in a cat with this form can be seen by the following signs:
Paralysis of the lower jaw, paws, torso develops as early as 2-3 days after the onset of symptoms.
In the paralytic form of rabies, the cat does not behave aggressively and does not react in any way to its owner.
The atypical form of the pathology is rare and characterized by a long course (up to several months). It is accompanied by lethargy, lethargy and depression. The cat eats poorly, gastrointestinal disorders (diarrhea, constipation, vomiting) may occur. Atypical rabies is accompanied by emaciation, convulsive trembling, muscular atrophy.
What to do if rabies is suspected?
If there are serious reasons to believe that a cat may be infected, Immediately Take the following measures:
- Complete avoidance of contact with the animal Isolate the cat completely and keep it completely isolated (in separate quarters);
- If the cat has bitten or scratched your skin, wash the wound immediately with mild soap and water;
- Go to a veterinarian and consult with a specialist about the pet's symptoms.
Important! Neglecting the above recommendations is fraught with rabies virus infection.
Diagnosis
As already emphasized, it can be very difficult to accurately determine that a cat is infected with rabies. In most cases, the veterinarian will only take concrete action when he or she has analyzed the pet's symptoms and concludes that the pet has something else but not rabies virus.

Otherwise, the veterinarian chooses a wait-and-see tactic until he finds the death of the animal. Only then does the vet proceed to examine the animal's brain tissue to find out whether it contains Babes-Negri cells. If the test is positive, all those who have previously been in contact with the cat are prescribed appropriate therapy.
As for drugs that would rid a pet of rabies, so far mankind has not invented them.
Sources of rabies
Rabies in cats – a viral disease, runs in an acute form and with a fatal outcome. Rabies affects all animals, as well as humans. This infection is manifested by nervous disorders and behavioral disorders. Cases of rabies are registered in wild and domestic animals everywhere, except in Australia and New Zealand, as well as in the British Isles, where strict quarantine measures have eliminated the infection. Due to the fact that rabies is carried by wild animals, the movement of which across territories cannot be restricted, the disease occurs in many countries.
The rabies virus is bacilliform and belongs to the lyssavirus genus, which can affect insects, all warm-blooded animals, including birds, and even plants.
The main sources of rabies infection for domestic cats can be:
- Wild animals. On homestead plots, in cottage communities, in the countryside a domestic cat can meet foxes, hedgehogs, mice, rats, squirrels, moles, otters; in the south – bats, which can infect a cat with rabies. It is advisable not to bring wild animals home, including those picked up in the city, as it is a great risk.
- Stray cats and dogs. Street animals often get rabies.
- Pets. Cats and dogs with this infection are dangerous to others.
- Infected surfaces. Surfaces on which the saliva of sick animals has been left can be a source of rabies virus in cats, but not for long because the virus is unstable in the environment.
Risk groups
- Stray cats;
- Unvaccinated free-range domestic cats;
- domestic unvaccinated free-range cats going out to the countryside or dacha, even those that are supervised on the property;
- Household free-range cats that have not been revaccinated.
How cats get rabies
The rabies virus is found in the saliva of sick animals. When bitten, the virus enters the wound with the saliva. The virus "prefers" muscles, less often blood. In the muscles there is primary reproduction of the virus, then by peripheral nerves it travels to the brain, where it again undergoes reproduction and by motor nerves enters the salivary glands, less often – to the eyes.
It is impossible to control a cat on a free walk, because these animals love the most secluded places. Many of the felines are good hunters, so they attack rodents, moles and hedgehogs. All the more so because their biological cycles (nocturnal lifestyle) coincide. The cat enters the fray and can get deep bites with skin and muscle damage. This is how the virus enters the pet's body and infection occurs.
Cats are territorial animals and are often even better guardians than dogs. A cat will defend its home and land to the last moment, even from strange companions. There is no animal more terrible than an angry cat. In fights, a pet can be injured by teeth and claws from stray sick cats. Wounds serve as a "gateway" for the virus to enter the body. Bite wounds from sick dogs can also lead to rabies infection.
A domestic cat can be infected with rabies when saliva containing the virus comes into contact with damaged mucous membranes and skin. Very rare but probable cases of transmission are airborne, when the virus concentration in the air is very high.
Ways of infection
Scientists-rabiologists from around the world have concluded that the causative agent survives a short time outside the body of the host. You can become infected by direct contact with the saliva and other secretions of a sick animal. Most often – through a bite or saliva in a wound, scratch or mucous membranes. There have also been cases where pets living in private homes or in the countryside have become infected after sick animals have eaten from their bowls and left droplets of contaminated saliva on dishes or food. For example, hedgehogs often enter private households in search of food without fear. It is also very common for cats to contract rabies by eating sick rodents.
Once the virus enters a healthy body, it begins to reproduce and move along the nerve fibers that are in the salivary glands, intestines, mucous membranes. Subsequently, viral encephalitis (inflammation of the brain) occurs. It leads to changes in behavior, aggression or depression, paralysis, coma and death of the animal in the final stages of the disease.
The incubation period of rabies in cats can last from ten days to two months. During this time, the animal does not yet have pronounced symptoms, but can already be a carrier. The duration of this period depends on several factors: the amount of virus that has entered the body, the location of its entry, the depth of the wound, the overall immunity of the animal. Bites to the head and genitals are the most dangerous, since there are many nerve endings where the virus develops. After the first clinical symptoms of the disease, the cat does not live more than 7-8 days, except for the atypical form of rabies, which can last up to several months.
The risk group primarily includes stray and free-range cats. But, unfortunately, the answer to the question of whether a fully house/apartment cat can get rabies is positive. The virus can be contracted on the way to the vet, it can be "brought" from the street on the shoes of the owner.
Symptoms and signs of rabies in cats
The symptomatology of the disease depends on its stage. Stages of rabies in cats can overlap or rapidly replace each other.
- The first stage is the incubation period. It passes without visible symptoms, but the virus is already actively multiplying and moving along the fibers of the central nervous system. Symptoms at this stage are usually not noticeable, but almost every owner who knows his pet well can sense that something is wrong. The pet looks unusually quiet, lethargic, refuses food and favorite treats. Excessive caution and suspicion may appear in the behavior. The cat may be too silent, or conversely, meow often and without cause, with the pet's voice becoming muffled or hoarse.
- The second stage is prodromal. It lasts about a day and goes rapidly into the stage of agitation and aggression. At this stage, the owner may notice expressive and unexpected changes in the pet's behavior. Self-sufficient and unsociable cats suddenly become too friendly and even obtrusive. And sociable cats, on the contrary, become withdrawn and look for dark corners. Also, the animal may behave strangely when eating. After refusing a favorite treat, the pet may try to eat completely inedible things, such as a stone.
- The third stage is agitation or the frenzy that gives the disease its name. In cats, rabies occurs in a violent form much more often than in other animals. This phase can last up to a week, or the animal from the prodromal stage immediately goes into the stage of paralysis. During the agitation phase, the cat is the most dangerous, and the amount of virus particles in its body is the highest. The affectionate pet becomes irritable, extremely nervous and angry. An attack of aggression or hysteria may be provoked by a sudden sound or flash of light, a draft from an open door or a splash of water. In addition to injuries from claws and teeth, the cat carries another terrible danger – a high probability of transmitting the virus to humans. In addition to pronounced nervousness or aggression, the animal suffers from muscle spasms and has severe salivation. Also during this period, the cat can no longer eat or drink due to muscle spasm.
- The next stage is the so-called "mute" stage. After agitation, paralysis occurs, which manifests itself in chaotic, uncoordinated movements of the animal and convulsions. It leads to a fatal outcome.






